
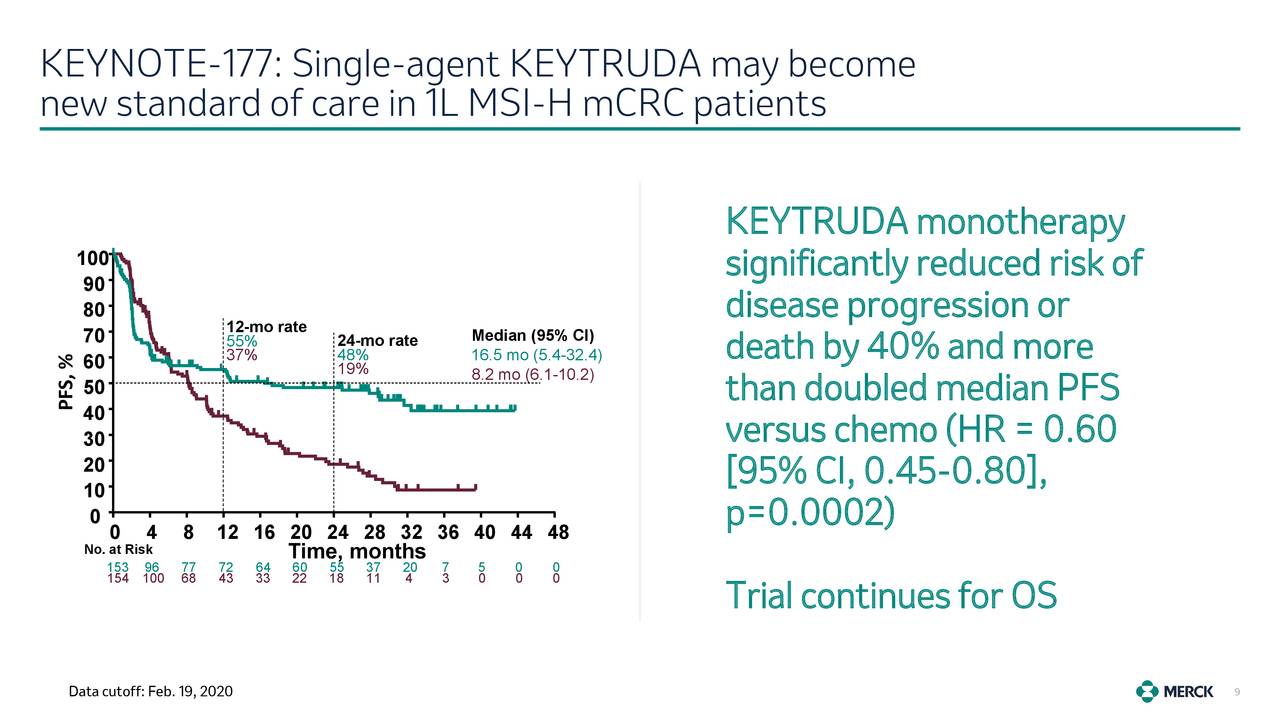
Advanced d-MMR/MSI-H CRCs are approximately 5% 12, 13.ĬRCs with d-MMR/MSI-H are characterized by the production of several cancer neoantigens, increasing tumor mutational burden (TMB) and immune cell infiltration, leading the tumor to be more sensitive to immunotherapy 14. About 15% of CRCs are dMMR/MSI-H these are more likely to have early-stage disease. However, there is no evidence that MSI-L CRC differs in their clinicopathological or molecular features from stable microsatellite tumors (MSS) 11. There are two distinct MSI phenotypes: high-MSI (MSI-H) and low-MSI (MSI-L), distinguished based on the type and number (≥ 40%) of microsatellites analyzed 11. Microsatellite instability (MSI) results from accumulations of high levels of single-base mismatches or short insertions and deletions in repetitive DNA tracts due to DNA mismatch repair system deficiencies 10. MMR genes inactivation can be due to several mechanisms (e.g., germ-line mutations or point mutations such as insertion and deletions), and this event can be involved in the tumorigenesis process 9. Their efficacy appeared closely related to mutations in mismatch repair (MMR) genes (MSH2, MSH6, MLH1, PMS1, and PMS2), essential for recognizing and repairing DNA errors that occurred during its replication 6, 7, 8. In recent years, the development of immune-checkpoint inhibitors (ICIs) has led clinicians to explore their role in advanced CRC settings 5. Despite recent progress in defining tumor molecular profiles with more personalized therapeutic strategies, CRC remains the second leading cause of cancer-related deaths worldwide 1, 2, 3, 4. Nowadays, colorectal cancer (CRC) still represents the third most diagnosed malignancy. Modulating the CDX-2/CXCL14 axis in CDX-2-negative patients could help overcome primary resistance to immunotherapy. Although our study reports results on a small population, the prognostic role of CDX-2 in CRC seems confirmed and could drive a promising predictive role in defining the population more sensitive to immunotherapy treatment. Twelve patients received 1st-line pembrolizumab (11 CDX-2 positive and 1 CDX-2 negative) not reaching median PFS, while two patients (1 CDX-2 positive and 1 CDX-2 negative) received 3rd-line pembrolizumab reaching a median PFS of 10.8 months (95% CI, 10.8–12.1 p = 0.036).
Among CDX-2-negative patients, one achieved stable disease, while the other progressed rapidly (ORR: 100% vs 0%, p = 0.0005 DCR: 100% vs 50%, p = 0.02). All CDX-2-positive patients achieved a disease response, one of them a complete response. Median OS was NR in CDX-2-positive patients versus 2.17 months (95% Confidence Interval 2.17–18.7) in CDX2-negative patients ( p = 0.026). The median PFS was not reached (NR) in the CDX-2 positive group versus 2.07 months (95%CI 2.07–10.8) in CDX-2 negative patients ( p = 0.0011). The PFS rate at 12 months was 81% in CDX-2 positive patients vs 0% in CDX-2 negative patients ( p = 0.0011). The secondary endpoints were overall survival (OS), PFS, objective response rate (ORR), and disease control rate (DCR). The primary endpoint was the 12-month progression-free-survival (PFS) rate.
We retrospectively collected data from 14 MSI-H mCRC patients treated with ICIs between 20. Therefore, we investigated CDX-2 role as a prognostic-predictive marker in patients with mCRC MSI-H. Caudal-related homeobox transcription factor 2 (CDX-2) would seem to influence immunotherapy’s sensitivity, promoting the chemokine (C-X-C motif) ligand 14 (CXCL14) expression. Unfortunately, a patient’s subgroup did not benefit from immunotherapy. Immune checkpoint inhibitors (ICIs) showed efficacy in metastatic colorectal cancer (mCRC) with mismatch-repair deficiency or high microsatellite instability (dMMR-MSI-H).


 0 kommentar(er)
0 kommentar(er)
